Introduction
This article will consider the ongoing policy debate regarding asbestos management and public health in the UK. The article has two aims. First, it aims to provide an overview of the current policy context. Second, the impacts of non-traditional asbestos exposure on the experiences of mesothelioma patients and their families will be presented with reference to the findings of two studies. Implications for the policy community will be addressed.
What is asbestos and what is the risk?
Asbestos first began to be used commercially in the UK in the 1870s. It is a mineral resistant to high temperatures, valued for its use as a fire retardant and heat insulating material. The UK has a history of exceptionally high asbestos use, being the biggest importer of asbestos in Europe between 1920 and 1970 (Kameda et al., 2014). Although asbestos was banned in the UK in 1999, many buildings built before this date still contain asbestos. Indeed, the period prior to the ban included a significant post war building programme that saw the construction of many public buildings including schools and hospitals. The urgency of this programme meant that prefabrication, or system building, was widely used and many of these schemes relied on asbestos as a building material.
Asbestos is the UK’s number one cause of work-related deaths (UKATA, 2023). It is a carcinogenic material associated with several health conditions, including asbestosis, cancer of the lung, larynx and ovary and mesothelioma (IARC, 2012). Mesothelioma is an incurable cancer and is caused almost exclusively by exposure to asbestos. While mesothelioma is a global burden, the prolific usage of asbestos in the UK means it has the highest recorded rate of mesothelioma in the world (Bianchi & Bianchi, 2014; Peto et al., 2009).
Mesothelioma is a devastating disease with a high symptom burden. It also has unique information and support needs due to its aetiology, prognosis and associated financial and legal implications. While treatment is improving, mesothelioma remains incurable, with the majority of patients dying within 12 months of diagnosis (CRUK, 2019).
Since 1970, the annual number of deaths caused by mesothelioma has increased. There are around 2,500 mesothelioma deaths in Great Britain each year, ten times more than the annual number in the 1970s (HSE, 2023). As a result of the ban on using asbestos, the number of people diagnosed with mesothelioma following exposure through manufacturing or use of asbestos products should decline, consistent with the 15-45 year time lag between exposure and presentation of the disease. It is currently predicted that until 2030, mesothelioma will continue causing 2,500 deaths in Great Britain each year (HSE, 2023). The number of deaths is expected then to decline. Nevertheless, there is concern and growing evidence that ‘background’ exposure to asbestos that remains in our buildings will delay the hoped-for fall in mesothelioma incidence (Mesothelioma UK, 2023; Taylor et al., 2023).
Due to the historical use of asbestos in industries such as construction, asbestos mining and dockyards, the incidence of mesothelioma has typically been higher in men and in certain occupational groups, (HSE, 2023). However, exposure to asbestos that is now degrading in UK buildings means that the patient profile is changing. Asbestos remains present in 94 per cent of hospital trusts in England and 80 per cent of UK state schools (Morrin et al., 2019). It is therefore unknown how many people will continue to be harmed by asbestos in the future. Existing projections of asbestos-related disease rates do not take this type of exposure into account. For example, no data tells us how many children are at risk from asbestos-related diseases as a result of asbestos exposure in public buildings such as schools and leisure centres. However, some modelling suggests that nine times more pupils than education workers are likely to develop mesothelioma due to asbestos exposure in schools (Environmental Protection Agency, 1980). A more recent UK report estimated that between the years 1980-2017, the estimated number of UK mesothelioma deaths exposed to asbestos as school pupils ranged from 3,890-9,000 (JUAC, 2021).
Policy context
April 2022 saw the publication of a UK Parliamentary Work & Pensions Select Committee report into the Health and Safety Executive’s approach to asbestos management (HoC, 2022a). The report argued that the status quo was unacceptable and there was a risk to public health if nothing changed. They made several recommendations concerning future management of asbestos. These included 1) the development of a national asbestos register to ensure accurate records of asbestos in buildings and 2) gradual removal of asbestos over the following 40 years, prioritising buildings where people are most at risk, such as schools.
The UK Government rejected two key recommendations (HoC, 2022b). The reason given for the decision not to remove asbestos was based on the low risk of exposure where the in-situ asbestos is effectively managed. Importantly, however, the Government has based their response on evidence about the risk of asbestos that has been shown to be a serious underestimate.
The underestimate arises from the data used by the Government. Each year, the Health and Safety Executive (HSE) publishes statistics about the number of mesothelioma deaths by occupational group (HSE, 2023). It is therefore possible to look at the data for the teaching professional group and health professional group. It is this data collected by the Office for National Statistics (ONS) that was referred to as an indicator of risk for workers in hospitals and schools in the Government response (HoC, 2022b) to the Select Committee recommendations (HoC, 2022a). There are crucial flaws to this dataset and these are presented in Box 1. These flaws explain why the data creates an underestimate of the risk of mesothelioma to hospital and education workers.
Box 1: Limitations of the ONS data used to determine risk of mesothelioma following asbestos exposure in schools and hospitals
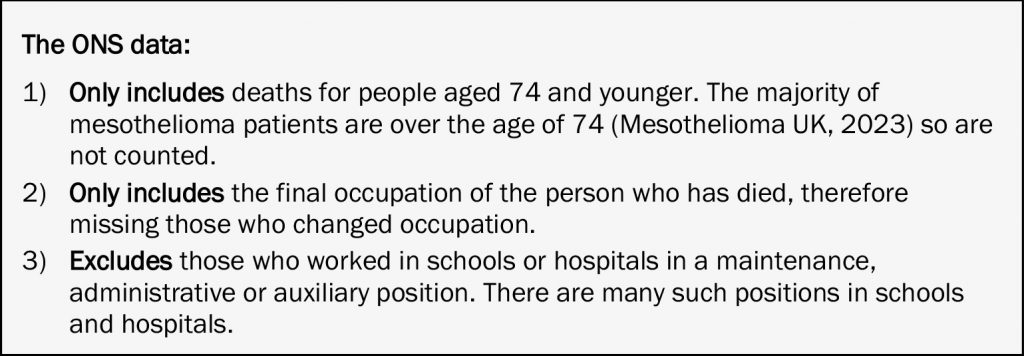
It follows that the ONS data used by the Government to justify its response to the Select Committee inquiry is likely to be a substantial underestimate of the number of people with mesothelioma following exposure to asbestos working in a school or hospital environment. This surmise is supported by evidence from Freedom of Information requests. For example, ONS data records deaths per year from mesothelioma as around seven per annum (pa) for health professionals and 23 pa for education professionals. By contrast the numbers of former health and education workers claiming mesothelioma-related benefit payments are around 65 pa and 70 pa respectively (Mesothelioma UK, 2023).
In addition to this underestimate of risk, there are further concerns about the Government’s response that in situ asbestos can be, and, more importantly, is being, effectively managed. In the first place, the poor condition of public buildings, such as schools and hospitals is well established (Cordery, 2022; NAO, 2023).
The first data analysis report following a survey of asbestos in UK buildings, was published in November 2022. The report highlights failings of current policy to manage asbestos in situ effectively and appropriately (ATAC & NORAC, 2022). The survey found that 71 per cent of the 710,433 items of asbestos found were damaged, evidencing the inadequacy of the current policy of in situ management. As the condition of buildings declines in the future, the extent of the damaged asbestos is likely to increase, further threatening public health.
Another concern is the nature of school environments, in which children behave as children do. Such wear and tear is above what is expected in a building that is not used by children every day. This is not accounted for in the Government’s in-situ management policy.
Amongst those who expressed disappointment at the UK Government’s rejection of the recommendation to remove asbestos from public buildings, was Charles Pickles, founder of the Airtight on Asbestos campaign. He said:
To put it bluntly, the UK has one of the worst asbestos legacies in the world – and our current lack of an informed strategy for dealing with this is shocking. For any project involving old buildings it will mean increased costs, delays, and even untimely deaths. Industry, campaigners, patient organisations and unions are united in their disappointment of this missed opportunity. (Politics.co.uk, 2022)
The European Commission has since launched a public consultation on a proposal to implement mandatory screening and registration of asbestos in buildings in Europe. Doing so will increase transparency and accessibility of information regarding asbestos for those at risk, such as construction workers and building occupants. This legislative initiative demonstrates a commitment by the EU Commission to address the risks of asbestos exposure, a commitment unmatched by the UK Government.
Despite the UK Government’s response to recommendations in the Select Committee report, debate regarding current policy for managing asbestos risk has maintained momentum. Campaigns, such as ‘Airtight on Asbestos’, led by Res Publica, and ‘Don’t let the dust settle’, led by Mesothelioma UK, have continued to raise awareness and lobby for change. In September 2023, Andrew Percy MP introduced a Private Members’ Bill to generate a national register of public buildings containing asbestos. In November 2023, a cost-benefit report was published by Mesothelioma UK in partnership with stakeholders. The report (Mesothelioma UK, 2023) estimates that in 2023 the total cost to the UK economy of asbestos-related diseases among former school and hospital workers was over £1.3 billion. Considering asbestos removal costs only, the benefits of removing asbestos from schools and hospitals over a 10-year period would outweigh the cost by a factor of three. This equates to a £3 million saving for every £1 million spent on removal. If the fabric of the building is made of an asbestos product, then demolition, rather than removal, is required. Cases where demolition is required are more expensive, reducing the cost benefit ratio to 0.85. This means that for every £1 million spent, the economy saves £850,000. The net cost to the Government remains relatively small at £2 billion over ten years. In addition, much of this rebuilding would have to take place in the near future anyway due to the poor condition of UK schools. There is now, therefore, a clear cost-benefit argument to removing asbestos from schools and hospitals.
Most recently, an All-Party Parliamentary Group meeting on occupational safety and health (asbestos) was held at the House of Commons (13 December 2023). The proceedings at this APPG indicated that the body of evidence and support to eliminate the risk of asbestos exposure for future generations is growing.
Here, we have summarised the current political context surrounding asbestos in UK public buildings. The next section will look at the human impact, presenting insights into the experiences of mesothelioma patients and their families following exposure to asbestos.
Human context
The Mesothelioma UK Research Centre has established a diverse portfolio of patient and carer experience research. This section draws on extracts and insights from two of these studies, each developing understanding into the experiences of mesothelioma patients exposed to asbestos in non-traditional environments: working in schools and hospitals. The two studies are:
1. The Mesothelioma Asbestos Guidelines Study (MAGS). This mixed methods study aimed to develop a critical account of the experiences of presentation, diagnosis, treatment and care for healthcare staff with mesothelioma. The study comprised:
- Stakeholder consultation.
- A literature review.
- Freedom of Information Requests.
- Seven qualitative interviews.
Findings showed that the current estimate of NHS workers diagnosed with mesothelioma is a gross underestimate and provided insights into the experiences of NHS workers diagnosed with mesothelioma. The study generated recommendations for clinical practice, future research and asbestos management. Further detail about the MAGS study can be found in related publications (Allmark et al., 2020a; Allmark et al., 2020b).
2. The Mesothelioma and Education Workers Study (MEWS) aimed to generate a critical account of the experiences of presentation, diagnosis, treatment and care for current and former school-based education workers with mesothelioma. The MEWS had three stages:
- Stakeholder consultation.
- A scoping review examining the experiences of school-based education workers who developed mesothelioma, including grey literature such as YouTube videos and blog posts.
- Analysis of national data, including Freedom of Information requests, to generate an indication of incidence of mesothelioma amongst school-based education workers.
Further detail about the MEWS study can be found in related publications (Taylor et al., 2022; Taylor et al., 2023).
The findings from these two studies provide insights into the changing profile of mesothelioma as people are exposed to asbestos in non-traditional environments. Those who develop mesothelioma in environments not yet recognised as high-risk are likely to have different experiences to those who have worked in industries known to be high risk. The following section draws on selected findings from both studies to explain why these experiences may differ.
Low index of suspicion
There is often immediate suspicion of mesothelioma when a person who presents with symptoms typical of mesothelioma has worked in an industry associated with asbestos exposure. People who have worked in industries not traditionally associated with asbestos exposure, such as hospitals or schools, are less likely to trigger timely suspicion. Similarly, as the industries known to be associated with asbestos exposure are dominated by men, women generally may be viewed by services with a lower index of suspicion. While there remains a need for statistical research to explore this index of suspicion further, qualitative data does suggest that this is the case.
They started asking me whether I’ve been exposed to asbestos and I was thinking no I don’t think so. I did you know and the chest surgeon … you know he didn’t, couldn’t believe a teacher would have it because I wasn’t in any of the industries known for this disease. (Source: YouTube Rosie Peters, patient, teacher (MEWS))
[We] had consultants that wouldn’t accept that she wasn’t suffering from something normal. Mesothelioma should be sort of kept at the back of everybody’s mind, I think. It’s not the first port of call, but when you’ve got something strange and you don’t know what it is you can’t rule it out. And the consultant I think said it couldn’t be some things because she hadn’t worked in industry. (Source: Interview with partner of health professional with mesothelioma (MAGS))
Eventually they said I’d have to go to [hospital] and have the lining of my lung sealed with talc. After I had the operation they asked me if I’d ever work with asbestos. I think until then they thought I had TB, that was the sort of that was the disease that was being suggested. (Source: Elizabeth Bradford, patient, teacher (MEWS))
Such low index of suspicion led to perceived delays in diagnosis as people with a work history not typically associated with asbestos exposure, and particularly women, presenting with symptoms were not expected to have been exposed to asbestos.
Distress and shock at diagnosis
It follows, that patients who have not worked in a known high-risk occupation are at more risk of high levels of distress and shock upon receiving their diagnosis.
You always think labourers get mesothelioma because they work so closely with these substances, but to be in a classroom day-in day-out with young children, it came as such a shock to us. (Source: Freddie Davis, husband of Pearl Davis, a teacher who died of mesothelioma a patient (MEWS))
I never for a second thought the job I loved and dedicated my life to, could give me a life limiting disease. (Source: Geoffrey Lee, patient, teacher (MEWS))
People unknowingly exposed to asbestos in an environment that was presumed to be safe spoke about a sense of injustice that they were not kept safe when working to educate or care for the public.
I think personally now, it’s ironic, that I’ve dedicated 44 years of my life, and you know, that dedication is what’s killing me now. It’s ironic really. (Source: Interview with health professional and patient (MAGS))
It follows, that people who receive a mesothelioma diagnosis following asbestos exposure in an environment not typically recognised as high-risk are likely to have additional psychological and emotional support needs. They may require more time of health professionals to understand and process the diagnosis.
Concern for others and on-going risk
Great concern, and for some anger, was experienced upon learning that that the asbestos risk remains in buildings such as hospitals and schools and the danger this continues to present. This can leave people with an additional enduring emotional burden.
What was also incredibly upsetting to Pearl was the idea that children may have been put at risk on those premises. It doesn’t bear thinking about.’ Source: Freddie Davis, husband of Pearl Davis a teacher who died of mesothelioma a patient (MEWS))
Mum was incredibly angry when she got her diagnosis as she was working in a school with asbestos. She worked … in primary schools with five-year-olds in reception. She hadn’t been able to protect them. Although Mum is now in the last weeks of her life, she is horrified that teachers and pupils continue to be exposed to asbestos in schools. (Source: Lucie Stephens, daughter of Sue Stephens a patient and teacher (MEWS))
Inequalities in accessing compensation
Mesothelioma is considered an industrial disease and therefore compensation is available to those who were exposed due to their employer’s negligence following the asbestos ban. Compensation can support patients to access non-NHS funded treatments to lengthen their lives. Compensation can also support families facing loss of earnings as a result of the disease.
Consultation with legal professional stakeholders during both the MEWS and MAGS highlighted that patients exposed to asbestos in an occupation not recognised as high risk are less likely to have a successful compensation claim. This relates to the point about index of suspicion made earlier. If a builder or carpenter developed mesothelioma then a lawyer usually has little problem in finding likely points of exposure. This is far more difficult if a teacher or health care professional develops mesothelioma. In these cases, it may be difficult to find specific cases of exposure that were due to negligence on the part of the employer and it is likely that the employer will contest the case. In general, lawyers will be reluctant to take these cases on and will only do so where there is a more than 50 per cent chance of winning. This generates an inequality between patients exposed in a high-risk industry and those exposed in an environment not yet recognised to be high risk, such as in a school or hospital.
The following extract demonstrates how hostile and tiresome claiming for compensation can be:
Now, what actually happened was that they [the lawyers representing the person with mesothelioma] were putting freedom of information requests and things to try and find out what they were doing at that period of time. And they [the employers] wouldn’t respond to us, so we got to the point of going to court. And one week before the court date, which they had put back a number of times, possibly even a couple of months actually, they suddenly delivered ten box files to [lawyer name]. And within one of the box files was a letter basically saying on a certain date, when [XX] was present, they were refurbishing the foyer, removing asbestos ceiling tiles. And they presented that to them and said got you. They said okay, and we settled out of court. They had the information, but they hid the information and they wouldn’t accept anything until we basically proved that they were doing something. (Source: Interview with a partner of health professional and patient (MAGS))
What does this mean for future policy?
The findings from these two studies give human context to the current political landscape. They provide insights into the changing profile of mesothelioma as people are exposed to asbestos in non-traditional environments. Public sector workers who develop mesothelioma in non-traditional environments may experience delayed diagnosis, additional emotional trauma and inequitable access to compensation. These people are therefore likely to have unique support and information needs.
There is an urgent need to improve the index of suspicion for mesothelioma when people present with symptoms and have an occupational history in non-traditional environments such as health care and education. We must challenge assumptions about asbestos exposure and risk, raising awareness of the risk in public buildings, such as schools and hospitals. To do this, it is essential that quantitative data accurately captures the past occupations of mesothelioma patients to remedy the current under-estimate. The identified flaws in the ONS data, used by the Government to justify the rejection of Select Committee recommendations, explain why there is a substantial underestimate of the number of people with mesothelioma following exposure to asbestos working in a school or hospital environment. The ONS data is not fit to inform decisions about asbestos management and risk. Relying on ONS data is putting the public at unnecessary risk. There is an urgent need to improve the quantitative data concerning the extent of mesothelioma amongst current and former NHS staff and education workers to inform policy.
If the UK Government wish to manage asbestos in situ, air monitoring must be considered an essential aspect of said management, especially in schools when there are additional concerns due to the unaccounted wear and tear caused by children. Air monitoring involves a process of measuring the concentration of asbestos fibres in the air to ensure that it is within safe limits. Routine air monitoring would provide assurance of a safe level for everyday use in buildings such as schools and hospitals. At present, air monitoring is only routinely used when asbestos is treated or removed. There are however further concerns about what the UK considers a safe level of airborne asbestos compared to other developed European nations. For example:
The UK’s current regime allows a ‘clearance level’ of airborne asbestos (0.01 f/cm3) which is five times greater than the ‘environmental limit’ allowed in France (0.005 f/cm3) and ten times greater than the acceptable ‘Occupational Exposure Limit’ in Germany (0.001f/cm) (https://www.airtightonasbestos.uk/_files/ugd/5e41e6_69da11396e5c44ffad18ab67d23d1953.pdf)
These observations raise serious questions about what the UK considers safe compared to other developed European nations. The UK must urgently reform its air monitoring standards.
Of course, if the EU Commission goes ahead with the proposed implementation of mandatory screening and registration of asbestos buildings, there will be challenges concerning readiness to proceed and logistical issues to consistent implementation across the EU. Hopefully, the UK Government can learn from the experience of our neighbours. Currently, safety in UK public buildings such as schools and hospitals is being compromised.
Conclusion
Asbestos remains a public health risk. This article provides insights into the changing profile of mesothelioma as more people are exposed to asbestos at work in occupations not traditionally associated with asbestos exposure. The changing patient profile can generate inequalities in care, including delays in diagnosis, increased support and information needs and a more challenging route to seeking compensation that can prevent access to non-NHS funded treatments. It is important to increase awareness of the risk of asbestos exposure to public sector workers. The possibility of non-traditional exposure should be highlighted for those taking an occupational history from patients with mesothelioma. Mesothelioma is a preventable, incurable cancer. Why, when we know the dangers, are public sector workers, school children and patients, being put at risk?
Dr Bethany Taylor, Mesothelioma UK Research Centre, Health Sciences School, University of Sheffield, Room B02, Barber House Annexe, 3a Clarkehouse Road, Sheffield S10 2LA. Email: Btaylor3@sheffield.ac.uk
Allmark, P., Tod, A. M., & Darlison, L. (2020a). MAGS: the healthcare staff mesothelioma asbestos guidance study. https://www.inspectas.co.uk/wp-content/uploads/2020/10/Meso-MAGS-Report-2020.pdf
Allmark, P., Tod, A. M., & Darlison, L. (2020b). Mesothelioma: are nurses being put at risk in the workplace? Nursing Standard, 35(12), 14-16. CrossRef link
ATAC & NORAC (2022). The first annual data analysis report into asbestos in UK buildings. Asbestos Testing and Consultancy & National Organisation of Asbestos Consultants. https://issuu.com/stevesadley/docs/atac_asbestos_report_nov2022?fr=sMDVkZTIwNzQwNjQ&mc_cid=e0c42f8746&mc_eid=9075920b1d
Bianchi, C., & Bianchi, T. (2014). Global mesothelioma epidemic: Trend and features. Indian Journal of Occupational and Environmental Medicine, 18(2), 82-88. CrossRef link
Cancer Research UK (CRUK) (2019). Survival for mesothelioma. Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/mesothelioma/survival
Cordery, S. (2022). Old buildings and out of date facilities are costing the NHS dear. British Medical Journal, 378. CrossRef link
Environmental Protection Agency (USA) (1980). Support document for proposed rule on friable asbestos-containing materials in schools: report no. 560/12-80-003. Washington. https://nepis.epa.gov/Exe/ZyPURL.cgi?Dockey=9100BENP.txt
Health and Safety Executive (HSE) (2023). Mesothelioma Statistics for Great Britain, 2023. Health and Safety Executive. https://www.coniac.org.uk/uploads/mesothelioma.pdf?v=1690278499
House of Commons, Work and Pensions Select Committee (2022a). The Health and Safety Executive’s approach to asbestos management. Sixth report of session 2021-2022. House of Commons. https://committees.parliament.uk/publications/21884/documents/162937/default/
House of Commons, Work and Pensions Select Committee. (2022b). The Health and Safety Executive’s approach to asbestos management: Government Response to the Committee’s Sixth Report of Session 2021–22. House of Commons. https://publications.parliament.uk/pa/cm5803/cmselect/cmworpen/633/report.html
International Agency for Research on Cancer (IARC) (2012). IARC Working Group on the Evaluation of Carcinogenic Risk to Humans. Arsenic, Metals, Fibres and Dusts. Volume 100C. International Agency for Research on Cancer. https://publications.iarc.fr/120
Joint Union Asbestos Committee (JUAC) (2021). Continuing Government failure leads to rise in school mesothelioma deaths: Are pupils and staff any safer today? Joint Union Asbestos Committee. https://the-juac.co.uk/wp-content/uploads/2021/07/Continuing-Government-Failure-leads-to-rise-in-school-mesothelioma-deaths-JUAC-REPORT-02-07-2021-FINAL1.pdf
Kameda, T., Takahashi, K., Kim, R., Jiang, Y., Movahed, M., Park, E., & Rantanen, J. (2014). Asbestos: use, bans and disease burden in Europe. Bulletin of the World Health Organisation, 92(11), 790-797. CrossRef link
Mesothelioma UK (2023). Clearing The Air: The costs and benefits of removing asbestos from UK schools and hospitals. Mesothelioma UK. https://www.mesothelioma.uk.com/downloads/clearing-the-air-the-costs-and-benefits-of-removing-asbestos-from-uk-schools-and-hospitals/
Morrin, M., Aldane, J., & King, H. (2019). Don’t Breath In: Bridging the Asbestos Safety Gap. ResPublica. https://www.respublica.org.uk/wp-content/uploads/2019/11/Asbestos-Report-Final.pdf
National Audit Office (NAO) (2023). Condition of School Buildings. National Audit Office https://www.nao.org.uk/reports/condition-of-school-buildings/
Peto, J., Rake, C., Gilham, C., & Hatch, J. (2009). Occupational, Domestic and Environmental Mesothelioma Risks in Britain: A Case-Control Study. British Journal of Cancer, 100(7), 1175-1183. CrossRef link
Politics.co.uk. (2022, July 25). The Government and HSE reject recommendations for reform of the UK’s asbestos management system. Politics.co.uk. https://www.politics.co.uk/opinion-former/press-release/2022/07/25/the-government-and-hse-reject-recommendations-for-reform-of-the-uks-asbestos-management-system
Taylor, B., Allmark, P., & Tod, A. (2022). The Experiences of Presentation, Diagnosis, Treatment and Care for School-Based Education Workers with Mesothelioma: A Scoping Review. International Journal of Nursing and Health Care Research, 5: 1342. CrossRef link
Taylor, B., Allmark, P., & Tod, A. (2023, April 18). The hidden danger of asbestos in UK schools: ‘I don’t think they realise how much risk it poses to students. The Conversation. https://theconversation.com/the-hidden-danger-of-asbestos-in-uk-schools-i-dont-think-they-realise-how-much-risk-it-poses-to-students-203582
UKATA (2023). Asbestos health statistics. UKATA. https://www.ukata.org.uk/library/asbestos-health-statistics