Abstract
International evidence suggests that homelessness and housing insecurity are associated with increased mortality, and for people that were formerly homeless, moving into secure housing is associated with decreased mortality. This paper explores the mortality among a cohort of formerly homeless people in Aotearoa New Zealand, who are now in Housing First, a programme designed to support housing security by providing wraparound support as well as stable housing. The Integrated Data Infrastructure was used, which links our de-identified cohort data with administrative data from various Aotearoa New Zealand government departments. Of the 390 in the Housing First cohort, 33 had passed away during the follow-up period, the majority of whom were men (63 per cent). The cohort that had experienced homelessness had an average age of death that was 18 years younger than that of a comparative sample from the Aotearoa general population. Notably, our findings also indicate that women utilising the Housing First programme tend to experience longer life expectancy compared to men. Our study underscores the need for continued support among people who have experienced homelessness due to their increased risk of mortality even after obtaining housing, highlighting the significance of early intervention and prevention.
Introduction
Homelessness in Aotearoa New Zealand (henceforth Aotearoa NZ to acknowledge the central place of Te Reo Māori and Te Ao Māori; Aotearoa is the Te Reo Māori name for the country) is a growing social concern. In Aotearoa NZ homelessness is defined broadly, to include living situations where people with no other options to acquire safe and secure housing are: in temporary accommodation, sharing accommodation with a household, or living in uninhabitable housing (Statistics New Zealand, 2009). Using this definition, the estimated population of those experiencing homelessness rose from at least 41,000 in 2013 to 102,123 in 2018, and then to 112,496 in 2023 (Amore, 2016; Amore et al., 2021; Statistics New Zealand, 2024), with an overall population prevalence rate of 2.3 per cent. The increase in size of this population between 2013 and 2018 is partially due to subsequent analysis, which identified an additional 60,000 people living in uninhabitable housing, making this the most prevalent form of homelessness in Aotearoa NZ (Amore et al., 2021). There are strong, complex relationships between housing and health. Homelessness is linked to adverse health outcomes, including higher rates of preventable acute and chronic medical conditions, traumatic injuries, assaults, serious psychiatric disorders, mental health issues, and disability (Davies & Wood, 2018; Charvin-Fabre et al., 2020). Significantly, Māori, the Indigenous population of Aotearoa NZ, Pacific People, and migrants are at a greater risk of experiencing homelessness compared to Pākehā/New Zealand Europeans (Amore, 2016; Amore et al., 2021). This disparity is a direct consequence of historical and ongoing colonisation in Aotearoa NZ. Land loss and confiscation, and loss of economic power and infrastructure, have led to significant inequities in housing (Groot et al., 2011; Lawson-Te Aho et al., 2019). As a part of this vicious cycle, Māori are underrepresented in home ownership and overrepresented throughout the housing support system and in homelessness statistics (Ministry of Housing and Urban Development, 2014; Houkamau & Sibley, 2015; Varona et al., 2021).
There is international evidence showing that the experience of homelessness is a risk factor for premature mortality (O’Connell. 2005; Hwang et al., 2009; Aldridge et al., 2019; Seastres et al., 2020). Adults who experience homelessness have mortality rates three to four times that of the general population (O’Connell, 2005). Additionally, almost one-third of these deaths are determined as preventable with timely and appropriate healthcare (Morrison, 2009; Henwood et al., 2015). There is evidence indicating that transitioning from homelessness to stable housing is linked to a decreased risk of mortality (Metraux et al., 2011). However, the literature on the influence of housing on health disparities, including mortality rates, remains unclear (Henwood et al., 2015).
Housing First (HF) is a support model designed for people experiencing homelessness with a high level of complex needs (Tsemberis et al., 2004). The HF approach involves supporting people unconditionally to access permanent housing and concurrently providing comprehensive support services, known as wrap-around support (Tsemberis et al., 2004; Tsemberis, 2011). Globally, HF has demonstrated its effectiveness in providing housing stability and improved social, health, and justice outcomes compared with usual services, such as shelters or emergency housing (Groton, 2013; Patterson et al., 2013; Aubry et al., 2016; Aquin et al., 2017; Rezansoff et al., 2017; Baxter et al., 2019). Across Aotearoa NZ, HF has yielded substantial positive outcomes for people experiencing homelessness, including enhanced overall well-being, reduced use of acute services such as emergency department usage, reduced rates of interactions with the justice system, and improved levels of income (Ombler et al., 2024; Fraser et al., 2023). However, post housing, their outcomes still differ substantially from the general population, showing the lasting impact and disadvantages of having experienced homelessness. This paper conducts a survival analysis for individuals housed by a HF programme in Aotearoa NZ. This programme, The People’s Project (TPP) was Aotearoa NZ’s first large-scale HF programme, established in 2014 as a response to growing visible homelessness on the streets of Kirikiriroa-Hamilton (a city in the north island of Aotearoa NZ) (Irvine & Sherson, 2021). TPP is driven by a local mental health non-governmental organisation (NGO), in partnership with Waikato-Tainui (the local Māori iwi/tribe); local council; local businesses; and government agencies including Health, Social Development and Corrections (Irvine & Sherson, 2021).
The work of TPP has been described in more detail in our previous papers (Pierse et al., 2019; Ombler et al., 2024; Fraser et al., 2021). Briefly, the programme aligns with HF core principles, prioritises people living without shelter, in emergency housing, or shared accommodation without secure tenure, for 12 months or more in the last three years, and who have a high level of complex needs. Housing is provided through working with public housing (government or community housing providers, paying an income-related rent set at 25 per cent of income) or directly with private landlords and an Accommodation Supplement. A multidisciplinary team deliver support according to people’s priorities, using intensive case management, with a staff ratio of 1:20, when possible. However, central government funding of TPP was limited during the timeframe for this analysis which may have reduced staff availability and the programme’s effectiveness (Tsemberis, 2011; Nelson et al., 2014). As there is very limited research on the links between homelessness and mortality in Aotearoa NZ, this paper seeks to provide a description of the mortality rates within a Housing First cohort, and how that differs to the general population. In addition, we seek to contribute to the international HF literature by comparing within the HF cohort (e.g., by gender and ethnicity).
Methods
We used survival analysis to study the mortality rates of the 390 formerly homeless TPP clients who were housed using the HF programme, 33 of whom passed away before 12 December 2022. Using the Integrated Data Infrastructure (IDI), we compared the mortality rates of the TPP participants with a random general population (GP) sample (n=33,195) from the resident population of Aotearoa NZ. The GP sample is restricted by age to the range of the HF cohort and has been selected such that they do not include the HF cohort. The individuals from the HF cohort are tracked from the date of entry into housing (September 2014-June 2017) until either the event of death or 12 December 2022 (the point at which analysis for this paper ended). Similarly, the GP is tracked from 9 June 2016 (the median date of housing for the HF cohort) until the end of 2022 or the event of death. Demographic information was derived from a composite dataset provided by Statistics New Zealand (Stats NZ), also in the IDI. The IDI is a collection of administrative data sources for the population of Aotearoa NZ provided by government agencies, Census and official surveys from samples of the population, and data collected from some non-governmental organisations (NGOs), maintained and regularly updated by StatsNZ. The IDI allows for linking de-identified administrative data across a wide range of government service interactions for the 390 individuals in the TPP HF cohort, available for IDI linkage (Pierse et al., 2019). Ethics approval for this study was granted by the University of Otago Human Research Ethics Committee, reference number 16/049.
The survival analysis was conducted using statistical analysis software R Studio (R Core Team, 2023). The primary purpose of survival analyses is to estimate the time until an event (such as death, failure, relapse, etc.) happens, and to understand the factors that may influence this time-to-event outcome among the HF population (Rich et al., 2010). All analysis was done on de-identified records in a secure Data Lab environment, and the necessary privacy, confidentiality, and security measures for IDI research have been observed. Of relevance, counts under six are suppressed due to confidentiality requirements; this is indicated in our tables with an ‘S.’ Counts outputted are also randomly rounded to base 3. The HF and GP data come from the October 2022 Refresh of the IDI. We categorised age into age groups to examine the association between demographic variables of the HF and GP cohorts using Fisher’s exact and Pearson’s Chi-squared tests. We utilised hazard functions and Kaplan-Meier survival curves for descriptive analyses, examining the timing and incidence of death post-move to housing. Additionally, a Cox proportional hazards regression model was applied to assess the association between demographic characteristics (gender, ethnicity, and age) of the HF participants and their risk of death following the transition to housing. To determine the model fit, goodness-of-fit tests (likelihood ratio, Wald, and score (log-rank)) were used.
Results
Acknowledgement of the Cohort
Before presenting the results of our analyses, we wish to acknowledge those who passed away in the cohorts, and the impact of these deaths on their families, friends, and wider communities. In our partnership with TPP, we have been able to see the impact this has on staff, and all of the work they do to support their clients and wider community as people pass. We have been moved by the support that TPP provide, such as facilitating final road trips to the beach, farewelling relatives in other cities, and coming together for a final favourite meal (personal communication, April 24, 2024). Last year, TPP teams came together for a Matariki (Māori new year) event to acknowledge the people they had worked with who had passed away in the past year. TPP kaimahi (team members) gathered on the banks of Lake Karapiro on the Waikato River, launching a raft with woven harakeke (flax) flowers and calling out the names of those who had died, as shown in Figure 1.
Figure 1: Harakeke flowers being released

Our analysis comprises a total of 390 people in the HF cohort, 33 (approximately eight per cent of this cohort) of whom passed away up to 12 December 2022. The comparative cohort consisted of 33,195 people from the GP, of whom 1,029 passed away during the same time period (approximately three percent). The study spans a cumulated total risk time of 7.04 years. Table 1 describes the demographic characteristics of the HF cohort and the GP comparison group. The average age of death for the HF cohort is 44 years old, compared to 62 years old for the GP. Elevated mortality rates were identified in the 45-64-year age group within the HF cohort, and a higher prevalence of deaths was observed among males compared to females (p<0.05) for those housed by HF. Amongst the GP sample, the mortality trend is similar with a lower prevalence of deaths observed among females (p<0.01). Approximately 73 per cent of those in the HF cohort who passed away were Māori (71.5 per cent of the overall HF cohort were Māori).
Table 1: Demographics for Housing First and the General Population
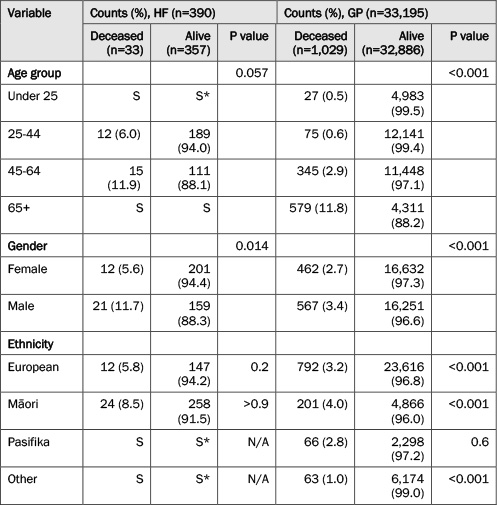
Note: p values were calculated using Fisher’s exact test and Pearson’s Chi-squared test. S=suppressed if counts are <6 and percentages are from suppressed counts. S*=Secondary suppression if the suppressed count (S) can be easily calculated. The numbers are randomly rounded to base three for confidentiality reasons. Percentages are reported by row, e.g., of the HF women, 5.6 per cent passed away.
Figure 2 illustrates the consistently higher survival probability throughout the study for the GP sample compared to the HF cohort. After two years of being housed, the survival probability for the HF cohort was 0.98, slightly lower than the 0.99 observed in the GP. Due to the steeper mortality gradient seen for the HF cohort, after five years of being housed, this HF group demonstrated a lower survival probability of 0.93 while the GP five-year survival probability was 0.98. Our Cox proportional hazard model demonstrates that the HF cohort had a five-year mortality risk of 2.79 times that of the GP population over the same time period (p<0.001).
Figure 2: Kaplan Meyer Graphs for Housing First and General Population
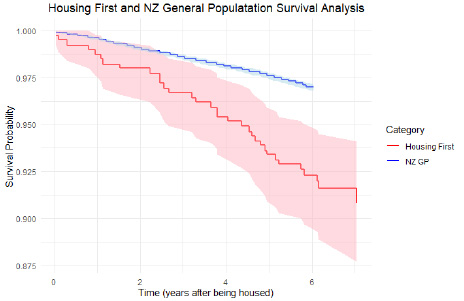
Figure 3 demonstrates the survival probability within the HF cohort stratified by gender.The survival curves for women and men initially followed a similar trajectory, indicating comparable survival experiences. However, a notable divergence in the curves became evident around the time point of 2.5 years. From this point onward, women exhibited a consistently higher survival probability compared to men. After five years of being housed, women demonstrate a relative stable survival probability of 0.97 compared to men at 0.89. The HF women’s survival probability is much closer to the women in the GP group at this time point (0.98) compared to the male HF-GP analyses. Furthermore, the univariate Cox proportional hazard model (Table 2) reveals a significant gender-based difference, where men have a hazard ratio of 2.38 compared to women (p<0.05). In the multivariate model, the risk remains high but not significant, with men having twice the risk of mortality compared to women (p=0.07). The goodness-of-fit tests show a significant difference in survival times and that the predictors contribute significantly to the model fit.
Figure 3: Kaplan Meyer Graphs for Housing First between genders
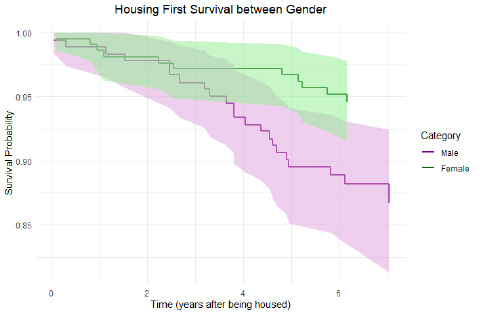
Table 2: Cox proportional hazards regression analysis for Housing First only
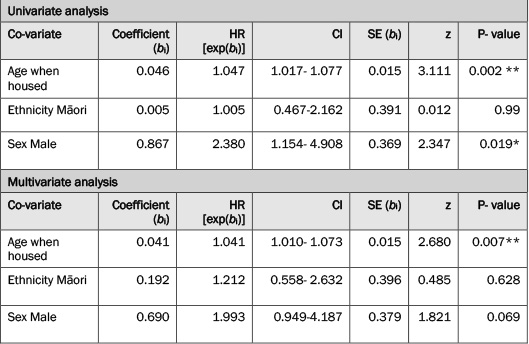
Note: * denotes statistical significance at the p<0.05 level, ** at the p<0.01 level. Goodness-of-fit tests for the multivariate analysis: Likelihood ratio test (χ² = 13.31, df = 3, p = 0.004), Wald test ((χ² = 12.8, df = 3, p = 0.005), Score (Log-Rank) test (χ² = 13.44, df = 3, p = 0.004).
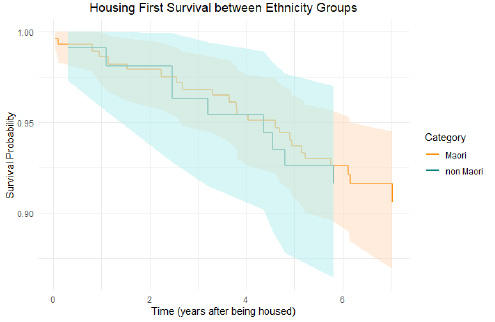
Figure 4 demonstrates the survival probability for the HF cohort stratified between Māori and non-Māori. At the two-year point, both Māori and non-Māori are at equal survival probabilities at 0.98. After five years, non-Māori have a survival probability of 0.93 whilst Māori have a survival probability of 0.94. In the univariate and multivariate models, the hazard ratio is respectively 1.00 (p=0.99) and 1.21 (p=0.63) for Māori. Both the univariate (HR=1.047, SE=0.0146, p<0.001) and multivariate models (HR=1.04, SE=0.015, p<0.01) show a statistically significant association between older age at the time of being housed and elevated risk of mortality.
Figure 4: Kaplan Meyer Graph for Housing First Ethnicities
Discussion
This paper presents the data of 390 people with unique stories and experiences of homelessness. Combining these individual stories into meaningful trends is important for understanding how people experiencing homelessness can be better supported to live long, healthy lives. This paper is the second in Aotearoa NZ to conduct a survival analysis to describe the rate of mortality amongst people who have experienced homelessness, reflecting similar findings to the first, which detailed a thirty-year shorter life expectancy for those experiencing homelessness, compared to the general population (Charvin-Fabre et al., 2020). Our paper extends these findings by investigating mortality in the years after being housed, and by gender and ethnicity. Our analyses show that the HF cohort had a higher mortality rate than the GP, with an increasing gap in the mortality gradients. While the comparative HF and GP cohorts were similar in age, the HF cohort passed away at a significantly younger age (on average 18 years younger), with elevated mortality particularly at ages 45 to 64 years, compared to the GP, for whom most deaths occurred over 65 years of age. An unexpected finding was a gender effect. While women had a higher survival rate in both cohorts, in the HF cohort, the survival rate for women after five years (0.97) is very similar to the survival rate of the GP (0.98). This is in contrast to the survival rate of men in the HF cohort, which is much lower at 0.89. These findings may suggest that HF solutions to homelessness—such as extended models of care—are particularly effective for women, where we see a considerable improvement in their survival rate from their second-year post-housing onwards, combined with forthcoming research which will show a post-housing reduction in healthcare interactions for women in this same cohort. They also suggest that ensuring timely access to permanent, secure, housing and other support services for women needs to be a priority in Aotearoa NZ. However, our analyses do not account for entry time into HF or the nature and severity of homelessness experienced, all of which may differ by gender, as may the individual vulnerability to impacts of homelessness.
The finding that the HF cohort had higher mortality than the GP supports international research which shows higher rates of mortality amongst people who have experienced homelessness compared with the general population (Hwang et al., 2009; Henwood et al., 2015; Stenius-Ayoade et al., 2018; Aldridge et al., 2019; Seastres et al., 2020; Tinland et al., 2021). These findings are also consistent with a previous analysis of cause of mortality in people who have experienced homelessness in Aotearoa NZ, which showed a 30-year reduced life expectancy in this population (Charvin-Fabre et al., 2020). Their analysis also showed that three quarters of the deaths would have been amenable to timely and effective healthcare interventions. In our study, the survival probability rate for the HF cohort had its biggest decrease in the fourth-year post-housing, demonstrating that health problems among people who were formerly homeless continue to impact even after people have been stably housed. Homelessness is often a symptom of long histories of poverty and discrimination in housing, often following childhoods marked by adversity (Piat et al., 2015; Kozloff et al., 2016). Experiencing poverty has profound impacts on health, through experiences including lack of access to healthcare and education, conditions of work and leisure, and the stresses associated with deprivation (Marmot et al., 2008). Homelessness further exacerbates these inequities, and therefore, increases risks of health problems. The high burden of illness associated with poverty can be reduced through policies and programmes that reduce these inequities, particularly when they address inequities early in life (Marmot et al., 2008). In Aotearoa NZ, thanks to ambitious child poverty targets set in 2018 that aim to halve child poverty (to reach only ten per cent of all children) by 2028 (Child Poverty Reduction Act, 2018), there are many initiatives that aim to reduce the health impacts of child poverty from the level of services, community and government, many of which are outlined in the 2022 Child Poverty Monitor Technical Report (Duncanson et al., 2022). These supports align with existing evidence in housing and homelessness research, underscoring the necessity of early and continuous support for people experiencing homelessness due to their heightened poor health status (Stergiopoulos et al., 2014).
Regarding gender differences in mortality, existing international research is mixed. Some studies report higher mortality among men, and some amongst women (Cheung & Hwang, 2004; Hwang et al., 2009; Morrison, 2009; Nielsen et al., 2011; Nusselder et al., 2013; Fine et al., 2023). Our results showed that men who had experienced homelessness had a lower survival probability than women. In particular, these gender differences only started to become apparent from the second-year post-housing. These findings suggest that there was a gender difference in survival outcomes from Housing First in this cohort. This difference may be explained by the experiences of homelessness that women tend to have, which are more often in overcrowded or inappropriate accommodation. These experiences may have less of an impact on people’s health compared to sleeping rough, which is more commonly experienced by men. Consequently, it is not entirely clear whether the gender difference in HF outcomes is due to the HF programme itself, though it evidences that despite the clear benefits of HF, the poor health outcomes that men face are persistent and unable to be sufficiently ameliorated by HF programmes, resulting in a higher mortality rate for men.
Research from Aotearoa NZ has shown that some of the main causes of mortality among people who were experiencing homelessness at the time of their death were cardiovascular disease and suicide; and 85 per cent were male and 15 per cent female, suggesting men may have greater personal vulnerability to the severest impacts of homelessness on health (Charvin-Fabre et al., 2020). Additionally, three quarters of deaths were deemed amenable to timely and effective healthcare intervention (Charvin-Fabre et al., 2020). A limitation of this study is that we were unable to assess the specific causes of mortality. This is due to the size of the cohort when considering comparisons of mortality rates between HF participants and the general population. Additionally, confidentiality constraints precluded release of this data. Future research could investigate the differences in mortality causes amongst larger HF cohorts and the general population, as well as other low-income populations. Our findings are also consistent with previous research demonstrating people who are older when experiencing homelessness are particularly at risk of early mortality (O’Connell 2005; Henwood et al. 2015; Tinland et al. 2021). In our study, the older a person was when they were housed, higher the risk of mortality. However, further research is needed to investigate the differing effects of homelessness based on age in Aotearoa NZ.
While there was no statistically significant ethnicity effect on mortality, there was a large over representation of Māori in the HF cohort (around 70 per cent compared to around 15 per cent in the GP cohort). Of Māori in each cohort, there was a higher proportion who passed away in the HF cohort than in the GP (8.5 per cent compared to 4.0 per cent, see Table 1). This statistic reflects the ongoing role of colonisation in determining access to housing (Kake, 2016; Lawson-Te Aho et al., 2019), as well as the ongoing effects of structural racism in the health system impacting the timely and effective provision of preventative and/or acute health support (Harris et al., 2018). To address these inequities in housing and health, structural changes must be made to the current housing and health systems, and enable equitable outcomes.
This study provides important evidence to inform strategies to address the mortality risk associated with homelessness in Aotearoa NZ. Our findings, alongside previous evidence of the higher lifetime rates of hospitalisations and welfare benefit receipt in this cohort (Ombler et al., 2024; Fraser et al., 2023; Pierse et al., 2022) suggest that interventions that promote equitable access to health and wellbeing measures for populations at greater risk of homelessness is warranted, as early intervention may have resulted in longevity rates closer to the general population for this cohort. Upstream of that, we also advocate for provision of improved (timely, effective, appropriate) prevention strategies—both universal and targeted for groups most at-risk, across sectors that influence health and housing-related outcomes. Additionally, the results highlight the need for ongoing specialist support for people experiencing homelessness in this country, even after they are stably housed (Henwood et al., 2015). Providing access to housing alone is unlikely to have improved mortality outcomes for this cohort (Ombler et al., 2024). The ongoing wraparound support and stability provided by Housing First programmes can improve quality of life, as well as facilitate community and whānau connectedness, providing dignity in death for those who are facing these very real mortality outcomes (personal communication, April 11, 2023). Importantly, we also continue to advocate for greater prevention of homelessness and poverty, to lessen these mortality outcomes in the first place.
We acknowledge the people who are discussed in this paper, each of whom had their own unique story to tell. We would also like to acknowledge the loss and grief faced by the whānau, friends, and communities of those who passed away. We are grateful to the staff of The People’s Project for their invaluable role. Without their permission and support, this work would not be possible. Ngā mihi nui.
This research was funded by a New Zealand Ministry of Business Innovation and Employment, Endeavour Fund research grant (UOOX1604). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of manuscripts.
These results are not official statistics. They have been created for research purposes from the Integrated Data Infrastructure, which is carefully managed by StatsNZ. For more information about the IDI, please visit https://www.stats.govt.nz/integrated-data/
Data was accessed with the permission of StatsNZ under their ‘five safes’ framework. All data are de-identified and only accessible via a secure connection from approved Data Labs. Data and results must be aggregated and anonymised in accordance with StatsNZ protocols. All results are checked for confidentiality by StatsNZ prior to their release from the secure environment. Data is available to those who have access to the IDI; it can be accessed in Aotearoa NZ by researchers working on public good projects.
Brodie Fraser, PO Box 7343, Newtown, Wellington, 6242, New Zealand. Email: brodie.fraser@otago.ac.nz
Aldridge, R.W., Menezes, D., Lewer, D., Cornes, M., Evans, H., Blackburn, R.M., Byng, R., Clark, M., Denaxas, S., Fuller, J., Hewett, N., Kilmister, A., Luchenski, S., Manthorpe, J., McKee, M., Neale, J., Story, A., Tinelli, M., Whiteford, M. … Hayward, A. (2019). Causes of death among homeless people: A population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Research, 4(49), pp. 1–17. CrossRef link
Amore, K. (2016). Severe housing deprivation in Aotearoa/New Zealand: 2001-2013. Wellington. http://www.healthyhousing.org.nz/wp-content/uploads/2016/08/Severe-housing-deprivation-in-Aotearoa-2001-2013-1.pdf
Amore, K., Viggers, H., & Howden-Chapman, P. (2021). Severe housing deprivation in Aotearoa New Zealand, 2018: June 2021 update. Wellington.
Aquin, J.P., Roos, L.E., Distasio, J., Katz, L.Y., Bourque, J., Bolton, J.M., Bolton, S-L., Wong, J.Y., Chateau, D., Somers, J.M., Enns, M.W., Hwang, S.W., Frankish, J.C., Sareen, J. (2017). Effect of Housing First on Suicidal Behaviour: A Randomised Controlled Trial of Homeless Adults with Mental Disorders. Canadian Journal of Psychiatry, 62(7), pp. 473-481. CrossRef link
Aubry, T., Goering, P., Veldhuizen, S., Adair, C.E., Bourque, J., Distasio, J., Latimer, E., Stergiopoulos, V., Somers, J., Streiner, D.L., & Tsemberis, S. (2016). A Multiple-City RCT of Housing First With Assertive Community Treatment for Homeless Canadians With Serious Mental Illness. Psychiatric Services, 67(3), pp. 275-281. CrossRef link
Baxter, A.J., Tweed, E.J., Katikireddi, S.V., & Thomson, H. (2019). Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health, 73, pp. 379-387. CrossRef link
Charvin-Fabre, S., Stolte, O., & Lawrenson, R. (2020). Amenable mortality within the New Zealand homeless population: We can do better! New Zealand Medical Journal 133(1527), pp. 26-38.
Cheung, A.M., & Hwang, S.W. (2004). Risk of death among homeless women: a cohort study and review of the literature. Canadian Medical Association Journal 170(8), p. 1243. CrossRef link
Child Poverty Reduction Act 2018. (N.Z.). https://www.legislation.govt.nz/act/public/2018/0057/18.0/whole.html
Davies, A., & Wood, L.J. (2018). Homeless health care: Meeting the challenges of providing primary care. Medical Journal of Australia, 209(5), pp. 230-234. CrossRef link
Duncanson, M., Roy, M., van Asten, H., Oben, G., Wicken, A., Tustin, K., McAnally, H., & Adams, J. (2022). Child Poverty Monitor 2022 Technical Report. Dunedin, NZ.
Fine, D.R., Dickins, K.A., Adams, L.D., Horick, N.K., Critchley, N., Hart, K., Gaeta, J.M., Lewis, E., Looby, S.E., & Baggett, T.P. (2023). Mortality by Age, Gender, and Race and Ethnicity in People Experiencing Homelessness in Boston, Massachusetts. JAMA Network Open, 6(8), p. E2331004. CrossRef link
Fraser, B., Chun, S., Pehi, T., Jiang, T., Johnson, E., Ombler, J., McMinn, C., & Pierse, N. (2023). Post-housing first outcomes amongst a cohort of formerly homeless youth in Aotearoa New Zealand. Journal of the Royal Society of New Zealand, 53(5), 656–672. CrossRef link
Fraser, B., White, M., Cook, H., Chisholm, E., Ombler, J., Chun, S., Tareha, H., & Pierse, N. (2021). Service usage of a cohort of formerly homeless women in Aotearoa New Zealand. SSM – Population Health, 15, 100842. CrossRef link
Groot, S., Hodgetts, D., Nikora, L., & Rua, M. (2011). Māori and homelessness. In T. McIntosh, & M. Mulholland (eds.), Māori and social issues. Huia Publishers. CrossRef link
Groton, D. (2013). Are Housing First Programs Effective? A Research Note. Journal of Sociology and Social Welfare, 40(1), pp. 51-64. CrossRef link
Harris, R.B., Stanley, J., & Cormack, D.M. (2018). Racism and health in New Zealand: Prevalence over time and associations between recent experience of racism and health and wellbeing measures using national survey data. PLoS ONE, 13(5). CrossRef link
Henwood, B.F., Byrne, T., & Scriber, B. (2015). Examining mortality among formerly homeless adults enrolled in Housing First: An observational study. BMC Public Health, 15(1). CrossRef link
Houkamau, C.A., & Sibley, C.G. (2015). Looking Māori Predicts Decreased Rates of Home Ownership. PLoS ONE, 10(3), p. e0118540. CrossRef link
Hwang, S.W., Wilkins, R., Tjepkema, M., O’Campo, P.J., & Dunn, J.R. (2009). Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ, 339, p. b4036. CrossRef link
Irvine, D., & Sherson, V. (Eds.). (2021). The Open Door: How The People’s Project Worked with Others to Make Homelessness Rare, Brief and Non-Recurring in Hamilton-Kirikiriroa. Hamilton-Kirikiriroa: The People’s Project.
Kake, J. (2016). Why are our people overrepresented amongst te pani me te rawakore?: Reflections on the root causes of Maori urban homelessness. Parity, 29(8), pp. 8-10.
Kozloff, N., Stergiopoulos, V., Adair, C.E., Cheung, A.H., Misir, V., Townley, G., Bourque, J., Krausz, M., & Goering, P. (2016). The unique needs of homeless youths with mental illness: Baseline findings from a housing first trial. Psychiatric Services, 67(10), pp. 1083-1090. CrossRef link
Lawson-Te Aho, K., Fariu-ariki, P.F., Ombler, J., Aspinall, C., Howden-Chapman, P., & Pierse, N. (2019). A principles framework for taking action on Māori/Indigenous Homelessness in Aotearoa/New Zealand. SSM – Population Health, 8(July), p. 100450. CrossRef link
Marmot, M., Friel, S., Bell, R., Houweling, T.A., & Taylor, S. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet, 372(9650), pp. 1661–1669. CrossRef link
Metraux, S., Eng, N., Bainbridge, J., & Culhane, D.P. (2011). The impact of shelter use and housing placement on mortality hazard for unaccompanied adults and adults in family households entering New York City shelters: 1990-2002. Journal of Urban Health, 88(6), pp. 1091-1104. CrossRef link
Ministry of Housing and Urban Development (2014). MAIHI Ka Ora – The National Māori Housing Strategy. Wellington.
Morrison, D.S. (2009). Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. International Journal of Epidemiology, 38(3), pp. 877-883. CrossRef link
Nelson, G., Stefancic, A., Rae, J., Townley, G., Tsemberis, S., Macnaughton, E., Aubry, T., Distasio, J., Hurtubise, R., Patterson, M., Stergiopoulos, V., Piat, M., & Goering, P. (2014). Early implementation evaluation of a multi-site housing first intervention for homeless people with mental illness: A mixed methods approach. Evaluation and Program Planning, 43, pp. 16-26. CrossRef link
Nielsen, S.F., Hjorthøj, C.R., Erlangsen, A., & Nordentoft, M. (2011). Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet, 377, pp. 2205-2219. CrossRef link
Nusselder, W.J., Slockers, M.T., Krol, L., Slockers, C.T., Looman, C.W.N., & van Beeck, E.F. (2013). Mortality and Life Expectancy in Homeless Men and Women in Rotterdam: 2001-2010. PLoS ONE, 8(10). CrossRef link
O’Connell, J.J. (2005). Premature Mortality in Homeless Populations: A Review of the Literature. Nashville.
Ombler, J., Jiang, T., Fraser, B., Nelson, J., McMinn, C., Hawkes, K., Atatoa Carr, P., Pehi, T., Aspinall, C., Bierre, S., Schick, K., Howden-Chapman, P., & Pierse, N. (2024). Five-Year Post-Housing Outcomes for a Housing First Cohort in Aotearoa, New Zealand. International Journal on Homelessness, 1–17. CrossRef link
Patterson, M.L., Rezansoff, S., Currie, L., & Somers, J.M. (2013). Trajectories of recovery among homeless adults with mental illness who participated in a randomised controlled trial of Housing First: A longitudinal, narrative analysis. BMJ Open, 3(9). CrossRef link
Piat, M., Polvere, L., Kirst, M., Voronka, J., Zabkiewicz, D., Plante, M.-C., Isaak, C., Nolin, D., Nelson, G., & Goering, P. (2015). Pathways into homelessness: Understanding how both individual and structural factors contribute to and sustain homelessness in Canada. Urban Studies, 52(13), pp. 2366-2382. CrossRef link
Pierse, N., Ombler, J., Chun, S., Fraser, B., White, M., Aspinall, C., McMinn, C., Howden-Chapman, P., Nelson, J., Hawkes, K., Jiang, T., & Atatoa-Carr, P. (2022). Two-Year Post-Housing Outcomes for a Housing First Cohort in Aotearoa New Zealand. European Journal of Homelessness, 16(2), 121–144. https://www.feantsaresearch.org/public/user/Observatory/2022/EJH_16-2/EJH_16-2_A5.pdf
Pierse, N., Ombler, J., White, M., Aspinall, C., McMinn, C., Atatoa-Carr, P., Nelson, J., Hawkes, K., Fraser, B., Cook, H., & Howden-Chapman, P. (2019). Service usage by a New Zealand Housing First cohort prior to being housed. SSM – Population Health, 8(June), 100432. CrossRef link
R Core Team (2023). R: A Language and Environment for Statistical Computing. https://www.R-project.org/
Rezansoff, S.N., Moniruzzaman, A., Fazel, S., McCandless, L., Procyshyn, R., & Somers, J.M. (2017). Housing First Improves Adherence to Antipsychotic Medication among Formerly Homeless Adults with Schizophrenia: Results of a Randomized Controlled Trial. Schizophrenia Bulletin, 43(4), pp. 852-861. CrossRef link
Rich, J.T., Neely, J.G., Paniello, R.C., Voelker, C.C.J., Nussenbaum, B., & Wang, E.W. (2010). A practical guide to understanding Kaplan-Meier curves. Otolaryngology – Head and Neck Surgery, 143(3), pp. 331-336. CrossRef link
Seastres, R.J., Hutton, J., Zordan, R., Moore, G., Mackelprang, J., Kiburg, K. V., & Sundararajan, V. (2020). Long-term effects of homelessness on mortality: a 15-year Australian cohort study. Australian and New Zealand Journal of Public Health, 44(6), pp. 476-481. CrossRef link
Statistics New Zealand (2009). New Zealand Definition of Homelessness. Wellington.
Statistics New Zealand (2024). 2023 Census severe housing deprivation (homelessness) estimates. https://www.stats.govt.nz/information-releases/2023-census-severe-housing-deprivation-homelessness-estimates/
Stenius-Ayoade, A., Haaramo, P., Kautiainen, H., Sunikka, S., Gissler, M., Wahlbeck, K., & Eriksson, J.G. (2018). Morbidity and housing status 10 years after shelter use — Follow-up of homeless men in Helsinki, Finland. European Journal of Public Health, 28(6), pp. 1092-1097. CrossRef link
Stergiopoulos, V., Gozdzik, A., O’Campo, P., Holtby, A.R., Jeyaratnam, J., & Tsemberis, S. (2014). Housing First: Exploring participants’ early support needs. BMC Health Services Research, 14(1). CrossRef link
Tinland, A., Loubiere, S., Cantiello, M., Boucekine, M., Girard, V., Taylor, O., & Auquier, P. (2021). Mortality in homeless people enrolled in the French housing first randomized controlled trial: a secondary outcome analysis of predictors and causes of death. BMC Public Health, 21(1), p. 1294. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11310-w
Tsemberis, S. (2011). Housing First: The Pathways Model to End Homelessness for People with Mental Illness and Addiction Manual. https://www.researchgate.net/publication/47669330
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing First, Consumer Choice, and Harm Reduction for Homeless Individuals With a Dual Diagnosis. American Journal of Public Health, 94(4), pp. 651-656. CrossRef link
Varona, G., Ogilvie, D., Darbyshire, Z., & Elumalai, V. (2021). Te pā harakeke : Māori housing and wellbeing 2021. Stats NZ, Wellington.